“Our results showed that in obesity, it is not the quantity but the quality of LDL that contributes to disease: “bad cholesterol” becomes worse due to obesity-associated inflammation. As a result, cholesterol delivery is shifted from normal to abnormal, so more cholesterol is retained in the arterial wall, ultimately forming plaques that occlude the blood flow,” explained corresponding author Shobini Jayaraman, Ph.D., a senior research scientist in pharmacology, physiology and biophysics.
Obesity has become an epidemic that is steadily spreading around the world, currently, estimates are that more than 40% of American adults are affected, and more than 9% of the population had severe Class 3 obesity in 2020 (this is the highest designation with a weight of 271+ pounds for a person that is 5’9” tall and a body mass index of 40+).
Obesity is a major risk factor for cardiovascular disease (CVD), diabetes, and certain cancers. Additionally, obesity often involves hyperlipidemia (elevated concentrations of fats/lipids in the blood), hypertension, oxidative stress, chronic inflammation, and diabetes which all have been shown to increase susceptibility to cardiovascular disease.
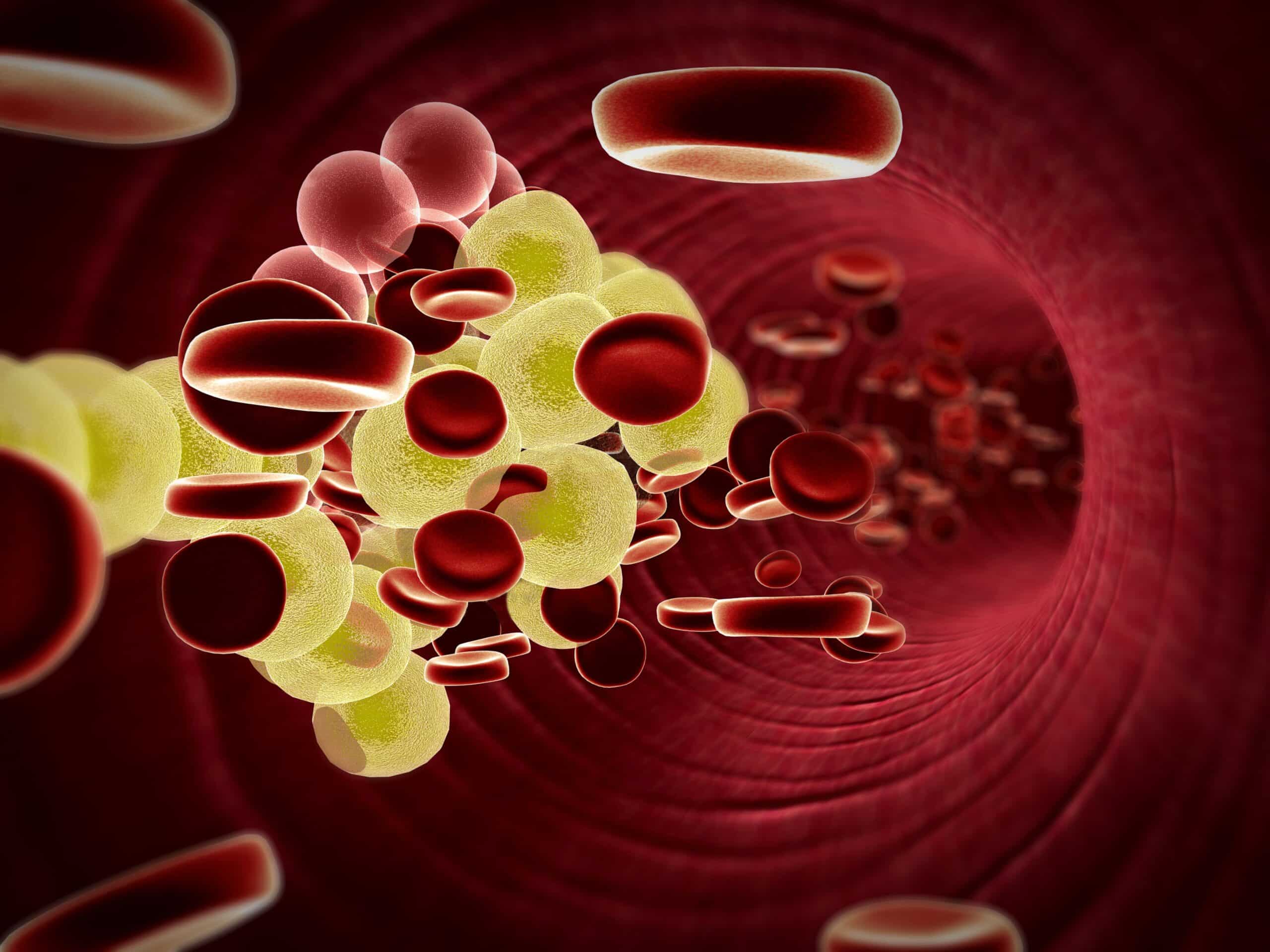
Nanoparticles called low-density lipoproteins (LDL) transport cholesterol in the blood. In moderation cholesterol is good and it is essential for normal cellular function. However, excess cholesterol can deposit and cause buildup in the arteries causing CVD, thus LDL has been called bad cholesterol.
For this study, researchers compared blood lipoproteins from those with severe obesity before bariatric surgery to lipoproteins from a control group of lean healthy subjects for either 6 or 12 months. Next lipoproteins’ interactions with three cell receptors important to LDL function were investigated, including the LDL receptor that directs uptake of cholesterol by the cells, and two scavenger receptors that can cause harmful accumulations of cholesterol. Then an assay was designed to quantify lipoprotein interactions with many extracellular matrix components, which included those that can promote harmful retention in the arteries leading to atherosclerosis. Additionally, LDL composition was analyzed using liquid chromatography and other biochemical methods in order to further explore nanoparticle charges and aggregations that influence LDL functions.
According to the researchers, in those with obesity before bariatric surgery, LDL particles were found to have become dysfunctional, and they were less efficient at delivering cholesterol cargo to LDL receptors. To add to this the LDL particles also tended to either preferentially stick to the arterial wall matrix or deliver cholesterol to scavenger receptors. However, during the first year after bariatric surgery, patients lost a significant amount of weight, obesity-induced inflammation subsided, and LDL quality progressively improved 6 and 12 months postoperatively. Despite the improvements, LDL quality did not reach the levels of the lean controls and neither did their BMI. Still, the LDL quality clearly aligned/correlated with the weight loss, and the closer weight was to healthy levels the better quality their LDL was, resulting in a decreased risk of CVD.
“This aberrant behavior stemmed from alterations in LDL biochemical composition induced by obesity-associated inflammation. These harmful changes contributed to increased risk of CVD in patients with obesity,” added Jayaraman.
“Our study shows that LDL quality continues to improve as a patient’s weight normalizes, suggesting that the risk of CVD continues to decline. This is promising not only for patients undergoing bariatric surgery but perhaps for many others who are overweight or obese and use various approaches to weight loss,” said senior author Olga Gursky, Ph.D., professor of pharmacology, physiology, and biophysics at the school.
It was noted that all clinical and some biochemical studies were performed by the Barcelona team led by Dr. Jose Luis Sanchez Quesada, the co-corresponding author of this study.