Once rare in developed countries, tuberculosis infections began increasing in 1985, partly because of the emergence of HIV, the virus that causes AIDS. HIV weakens a person’s immune system so it can’t fight the TB germs. In the United States, because of stronger control programs, tuberculosis began to decrease again in 1993 but remains a concern.
Many strains of tuberculosis resist the drugs most used to treat the disease. People with active tuberculosis must take several types of medications for many months to eradicate the infection and prevent the development of antibiotic resistance.
Symptoms
Although your body may harbor the bacteria that cause tuberculosis (TB), your immune system usually can prevent you from becoming sick. For this reason, doctors make a distinction between:
- Latent TB. In this condition, you have a TB infection, but the bacteria remain in your body in an inactive state and cause no symptoms. Latent TB, also called inactive TB or TB infection, isn’t contagious. It can turn into active TB, so treatment is important for the person with latent TB and to help control the spread of TB. An estimated 2 billion people have latent TB.
- Active TB. This condition makes you sick and in most cases can spread to others. It can occur in the first few weeks after infection with the TB bacteria, or it might occur years later.
Signs and symptoms of active TB include:
- Coughing that lasts three or more weeks
- Coughing up blood
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
Tuberculosis can also affect other parts of your body, including your kidneys, spine or brain. When TB occurs outside your lungs, signs and symptoms vary according to the organs involved. For example, tuberculosis of the spine may give you back pain, and tuberculosis in your kidneys might cause blood in your urine.
When to see a doctor
See your doctor if you have a fever, unexplained weight loss, drenching night sweats or a persistent cough. These are often signs of TB, but they can also result from other medical problems. Your doctor can perform tests to help determine the cause.
The Centers for Disease Control and Prevention recommends that people who have an increased risk of tuberculosis be screened for latent TB infection. This recommendation includes people who:
- Have HIV/AIDS
- Use IV drugs
- Are in contact with infected individuals
- Are from a country where TB is common, such as several countries in Latin America, Africa and Asia
- Live or work in areas where TB is common, such as prisons or nursing homes
- Work in health care and treat people with a high risk of TB
- Are children and are exposed to adults at risk of TB
Causes
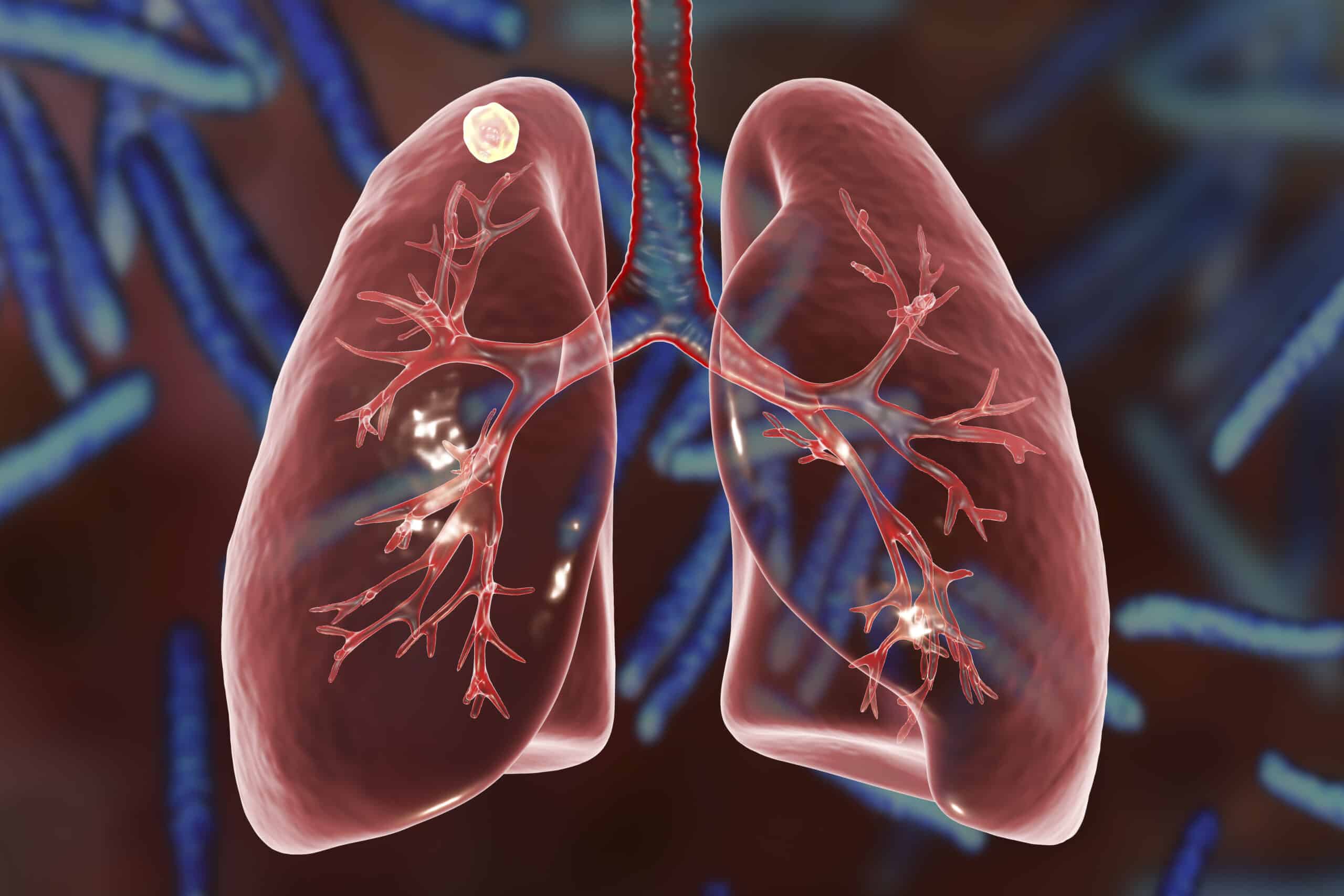
Tuberculosis is caused by bacteria that spread from person to person through microscopic droplets released into the air. This can happen when someone with the untreated, active form of tuberculosis coughs, speaks, sneezes, spits, laughs or sings.
Although tuberculosis is contagious, it’s not easy to catch. You’re much more likely to get tuberculosis from someone you live with or work with than from a stranger. Most people with active TB who’ve had appropriate drug treatment for at least two weeks are no longer contagious.
HIV and TB
Since the 1980s, the number of cases of tuberculosis has increased dramatically because of the spread of HIV, the virus that causes AIDS. Infection with HIV suppresses the immune system, making it difficult for the body to control TB bacteria. As a result, people with HIV are many times more likely to get TB and to progress from latent to active disease than are people who aren’t HIV positive.
Drug-resistant TB
Another reason tuberculosis remains a major killer is the increase in drug-resistant strains of the bacterium. Since the first antibiotics were used to fight tuberculosis more than 60 years ago, some TB germs have developed the ability to survive despite medications, and that ability gets passed on to their descendants.
Drug-resistant strains of tuberculosis emerge when an antibiotic fails to kill all of the bacteria it targets. The surviving bacteria become resistant to that particular drug and frequently other antibiotics as well. Some TB bacteria have developed resistance to the most commonly used treatments, such as isoniazid and rifampin.
Some strains of TB have also developed resistance to drugs less commonly used in TB treatment, such as the antibiotics known as fluoroquinolones, and injectable medications including amikacin and capreomycin (Capastat). These medications are often used to treat infections that are resistant to the more commonly used drugs.
Risk factors
Anyone can get tuberculosis, but certain factors can increase your risk of the disease. These factors include:
Weakened immune system
A healthy immune system often successfully fights TB bacteria, but your body can’t mount an effective defense if your resistance is low. A number of diseases, conditions, and medications can weaken your immune system, including:
- HIV/AIDS
- Diabetes
- Severe kidney disease
- Certain cancers
- Cancer treatment, such as chemotherapy
- Drugs to prevent rejection of transplanted organs
- Some drugs used to treat rheumatoid arthritis, Crohn’s disease, and psoriasis
- Malnutrition
- Very young or advanced age
Traveling or living in certain areas
The risk of contracting tuberculosis is higher for people who live in or travel to areas that have high rates of tuberculosis and drug-resistant tuberculosis, including:
- Africa
- Eastern Europe
- Asia
- Russia
- Latin America
- Caribbean Islands
Poverty and substance use
- Lack of medical care. If you receive a low or fixed income, live in a remote area, have recently immigrated to the United States, or are homeless, you may lack access to the medical care needed to diagnose and treat TB.
- Substance use. Use of IV drugs or excessive alcohol weakens your immune system and makes you more vulnerable to tuberculosis.
- Tobacco use. Using tobacco greatly increases the risk of getting TB and dying of it.
Where you work or live
- Health care work. Regular contact with people who are ill increases your chances of exposure to TB bacteria. Wearing a mask and frequent hand-washing greatly reduce your risk.
- Living or working in a residential care facility. People who live or work in prisons, homeless shelters, psychiatric hospitals or nursing homes are all at a higher risk of tuberculosis. That’s because the risk of the disease is higher anywhere there is overcrowding and poor ventilation.
- Living in or emigrating from a country where TB is common. People from a country where TB is common may be at high risk of tuberculosis infection.
- Living with someone infected with TB. Living with someone who has TB increases your risk.
Complications
Without treatment, tuberculosis can be fatal. The untreated active disease typically affects your lungs, but it can spread to other parts of your body through your bloodstream. Examples of tuberculosis complications include:
- Spinal pain. Back pain and stiffness are common complications of tuberculosis.
- Joint damage. Tuberculous arthritis usually affects the hips and knees.
- Swelling of the membranes that cover your brain (meningitis). This can cause a lasting or intermittent headache that occurs for weeks. Mental changes also are possible.
- Liver or kidney problems. Your liver and kidneys help filter waste and impurities from your bloodstream. These functions become impaired if the liver or kidneys are affected by tuberculosis.
- Heart disorders. Rarely, tuberculosis can infect the tissues that surround your heart, causing inflammation and fluid collections that may interfere with your heart’s ability to pump effectively. This condition, called cardiac tamponade, can be fatal.
Prevention
If you test positive for latent TB infection, your doctor may advise you to take medications to reduce your risk of developing active tuberculosis. The only type of tuberculosis that is contagious is the active variety, when it affects the lungs. So if you can prevent your latent tuberculosis from becoming active, you won’t transmit tuberculosis to anyone else.
Protect your family and friends
If you have active TB, keep your germs to yourself. It generally takes a few weeks of treatment with TB medications before you’re not contagious anymore. Follow these tips to help keep your friends and family from getting sick:
- Stay home. Don’t go to work or school or sleep in a room with other people during the first few weeks of treatment for active tuberculosis.
- Ventilate the room. Tuberculosis germs spread more easily in small closed spaces where air doesn’t move. If it’s not too cold outdoors, open the windows and use a fan to blow indoor air outside.
- Cover your mouth. Use a tissue to cover your mouth anytime you laugh, sneeze, or cough. Put the dirty tissue in a bag, seal it and throw it away.
- Wear a mask. Wearing a surgical mask when you’re around other people during the first three weeks of treatment may help lessen the risk of transmission.
Finish your entire course of medication
This is the most important step you can take to protect yourself and others from tuberculosis. When you stop treatment early or skip doses, TB bacteria have a chance to develop mutations that allow them to survive the most potent TB drugs. The resulting drug-resistant strains are much more deadly and difficult to treat.
Vaccinations
In countries where tuberculosis is more common, infants often are vaccinated with the bacillus Calmette-Guerin (BCG) vaccine because it can prevent severe tuberculosis in children. The BCG vaccine isn’t recommended for general use in the United States because it isn’t very effective in adults. Dozens of new TB vaccines are in various stages of development and testing.