Researchers are moving forward in the process of developing personalised treatment that is based upon a patient’s skin cell for diseases of the central nervous system. Advances have brought promise and hope increasing the expectation that such diseases may be improved via use of stem cell research and therapies. Stem cells can develop into just about any type of cell in the body. Previous studies conducted have shown that transplantation of neural stem cells reduces inflammation and can help the injured central nervous system heal.
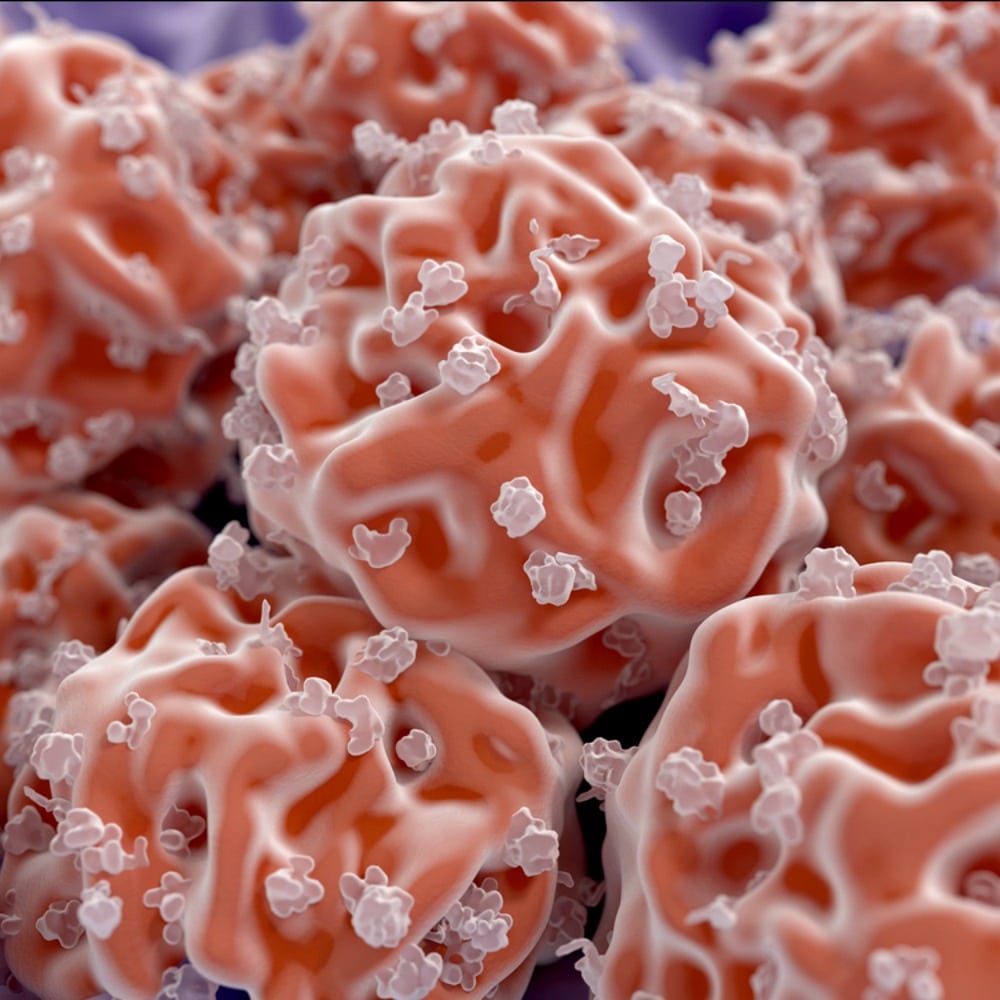
The body’s own immune system attacks the protective sheath around nerve fibres called myelin, causing disruption to signals sent around the spinal cord and brain in cases of multiple sclerosis. Immune cells involved causing the damage are macrophages called microglia which ordinarily rid the body of unwanted intruders. Symptoms of multiple sclerosis are varied and unpredictable and can include problems with balance, pain, mobility, and severe fatigue.
If a therapy could be developed it would be hindered by the fact that neural stem cells are sourced from embryos and can’t be obtained in quantities that would be large enough, there is also a risk that the body will see them as alien invaders triggering the immune response to destroy them. Possible solution could be use of induced neural stem cells that are generated by adult skin cells and reprogramming them into neural stem cells, these cells would be the patient’s own cells and less likely to trigger an immune response. This study has shown that this may be a viable option to repair some of the damage caused by multiple sclerosis.
Researchers discovered that chronic multiple sclerosis leads to significantly increasing the levels of succinate which is a metabolite that sends signals to microglia and macrophages tricking them into causing inflammation not only in cerebrospinal fluids but also peripheral blood in model mice. Transplanting directly into cerebrospinal fluids of induced neural stem cells and neural stem cells reprogramming of the microglia and macrophages turning them into good cells leads to a decrease in inflammation and subsequent secondary damage to the brain and spinal cord. Results of this study are suggestive of using a patient’s reprogrammed cells could provide a method of treatment personalised to the treatment of chronic inflammatory diseases including progressive forms of multiple sclerosis, which is promising as these cells are should be more available than convention neural stems cells with the added possible bonus of not carrying immune response.
This discovery was made by collaboration of researchers from diverse fields including cancer, mitochondrial biology, inflammation and stroke, regenerative medicine, and cellular reprogramming, without this multidisciplinary collaboration much of this research would not have been made possible, proving once more the importance of teamwork.