Despite the time and investment into Alzheimer’s disease, it still remains incurable, and this debilitating brain wasting disease kills hundreds of thousands of people every year. Currently scientists and drug makers test possible drug treatments by identifying those who are at an increased risk of developing the disease and then observing whether or not the candidate treatment in question will help to slow/prevent disease onset or not.
However, statistics show that 1 in 10 people will develop the disease after the age of 65, and 1 in 3 will develop the disease after the age of 85 which means that this observation can take years to decades to conduct, and this is a big part of the reason why even after nearly of century of studying this disease, progress is moving at a snail’s pace. Another challenge to trials is that participants must display symptoms of the disease to be eligible. Unfortunately the appearance of symptoms indicates that many brain cells have already died, and by that time it is typically too late for any treatments to have any significant effect on their symptoms.
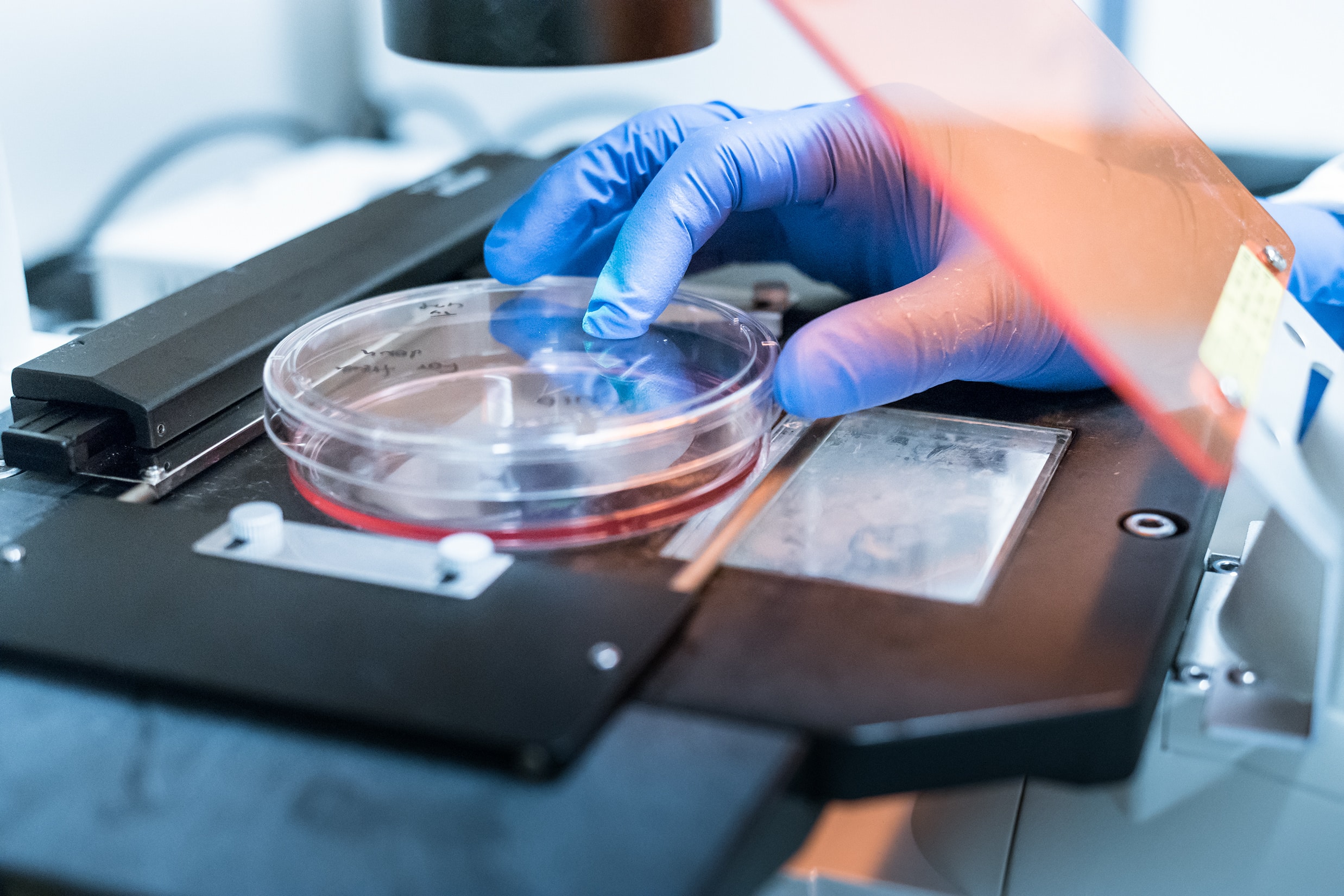
Recently a research team from Queen Mary University developed a new system to efficiently screen potential treatments for the disease that may be able to expedite the path for a cure, which is described in the Nature group journal Molecular Psychiatry. The study consisted of a cohort of people living with Down Syndrome who have a 70% increased likelihood of developing the disease as they carry an extra chromosome 21 that contains a gene that increases their risk. Hair cells were collected from the participants which were reprogrammed to become stem cells, then the stem cells were grown in a petri dish to become brain cells.
The research team observed a rapidly developing pathology that resembled Alzheimer’s disease in these brain-like cells, right down to the hallmark trio of indicators: progressive neuron death, amyloid plaque like lesions, and accumulations of tau protein tangles inside neurons. In this test environment 2 drugs were experimented with that are known to inhibit beta amyloid production which were applied to the new brain cells; after 6 weeks the drugs were found to have successfully prevented the onset of Alzheimer’s disease pathology.
It was noted that the 2 drugs used in these experiments had failed clinical trials for other reasons, and thus are not suitable treatments. But their system was able to demonstrate proof of concept for obtaining and developing cells to be used as a test environment that could be used as an Alzheimer’s disease drug testing platform for other preventative drugs in the future.
The team hopes that by creating lab controlled cellular environments that replicate human brain cells as the disease develops, the time it takes to test potential treatments could be decreased significantly, and thus the path to a cure could be diminished as well. In this study results were observed within 6 weeks, in the future if such an expedited timeline to determine the effectiveness of a drug saves many years of research, it could also save millions of lives and the suffering of those living with this horrible disease.
“This work represents a remarkable achievement, as this is the first cell-based system that has the full trio of Alzheimer’s pathologies, without any artificial gene over-expression,” said Queen Mary University of London Professor Dean Nizetic, who is also the lead author on the study. “This system opens up the prospect for screening for new drugs aimed at delaying or even preventing Alzheimer’s before neuronal death starts.”
The team also found evidence of the existence of a naturally functioning BACE2 gene that suppresses the disease which acts in a similar manner to tumor suppressing genes in cancer. Increased activity of this gene contributed to the slowing down and/or prevention of the disease in the tissues, this could in the future be used as a biomarker to determine the risk of developing Alzheimer’s disease, or as a possible new therapeutic approach by boosting its actions.
“Although it’s still early days, the system raises a theoretical possibility for further development as a tool to predict who might develop Alzheimer’s. The same stem cell process could be used on anyone’s hair follicles, the resulting brain cells of which may or may not then develop Alzheimer’s-pathology in the dish. The idea would be to catch the people at higher risk of early disease in a cell-based system, before it starts in a person’s brain and allow for the possibilities of individualized preventive interventions.”
Co-author Professor John Hardy added that although they are still a long way from reaching this goal, the potential development of a new human model of the disease “would be a great step forward.”
Carol Boys, Chief Executive of the Down’s Syndrome Association, said: “These are exciting results from an extremely eminent group of researchers and another small step towards a possible intervention and treatment for Alzheimer’s Disease. The Down’s Syndrome Association is delighted to have been able to support this brilliant work.”