In what may be a historic medical procedure, surgeons used an advanced form of stem cells to treat a patient with macular degeneration. The 60-year-old Japanese man with retinal disease is the first to receive stem cells derived from iPS-cell technology which reprograms donor cells into an embryonic state. IPS cells could make stem cells more attractive as a treatment while drastically reducing medical costs. Macular degeneration can lead to blindness, and doctors are hopeful that the new retinal cells will halt further progression of the disease in the patient.
Skin Cells Reprogrammed into Embryonic State
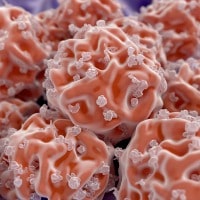
The creation of iPS cells begins with a donated sample of skin cells which are then genetically reprogrammed into embryonic cells. These embryonic cells have the unique ability to turn into any cell type and scientists are eager to use this technology to treat various diseases. In the case of the Japanese man, iPS cells were coaxed into developing into retinal cells that were transplanted onto the diseased retina.
Experiments were performed on Japanese women in 2014 using her own stem cells, and some successes have been accomplished. This procedure involves reprogramming self-donated skin cells but increases the risk of genetic abnormalities due to the fact that most patients are elderly. After one year despite these risks, the women fared well and the transplanted stem cells went on to fully develop into retinal cells.
The downside to donor iPS cells is they are not a genetic match for the patient and have a chance for immune rejection. But Nobel-prizewinning scientist Shinya Yamanaka, who is a pioneer in iPS stem cell research, makes the argument that banked iPS cells will be a match for most patients.
iPS Cell Banks Make Transplants Readily Available
Researchers in Japan plan on banking iPS cells from donors to reduce costs. The banked cells are then immediately ready for transplanting into patients. Without donor cell banks, the transformation of patients skin cells into iPS cells could take several months. In order for an iPS cell bank to be viable to the population, donor cells must be a match for patients. A cell match must pass a test involving certain proteins on the surface of donor cells, as the wrong match might trigger an immune rejection.
The team hopes that by 2018, cell lines created from 5 to 10 donors could match up to 50% of the population of Japan. After the pioneering surgery in Japan, researchers were hesitant to declare success. They must continue to monitor the patient’s transplanted retinal cells for any future abnormalities. With determination, they declared that this is only the beginning.