Now, new research by Canadian and Chinese scientists published in Nature outlines a method to marry these properties in a biodegradable gel. “Cartilage is tricky,” says senior author Dr. Hongbin Li, a professor in the UBC Department of Chemistry. “Articular cartilage repair represents an important medical challenge because naturally speaking, it doesn’t repair itself.
Biodegradable cartilage implants must strike a delicate balance in that they need to be both stiff and tough, like actual cartilage. Mechanically, when something is stiff, it resists being bent or deformed, but that usually means it’s brittle – when you bend it, it breaks, like glass. When something is tough, it resists breaking, even when you bend it, but it might be too soft to be useful in a joint, like jelly, or even just softer than actual cartilage. That’s the case with current implants that are made from proteins, which creates a mismatch between what the cells need and what’s being provided, says Dr. Li. This leads to the cartilage not repairing as well as it could.
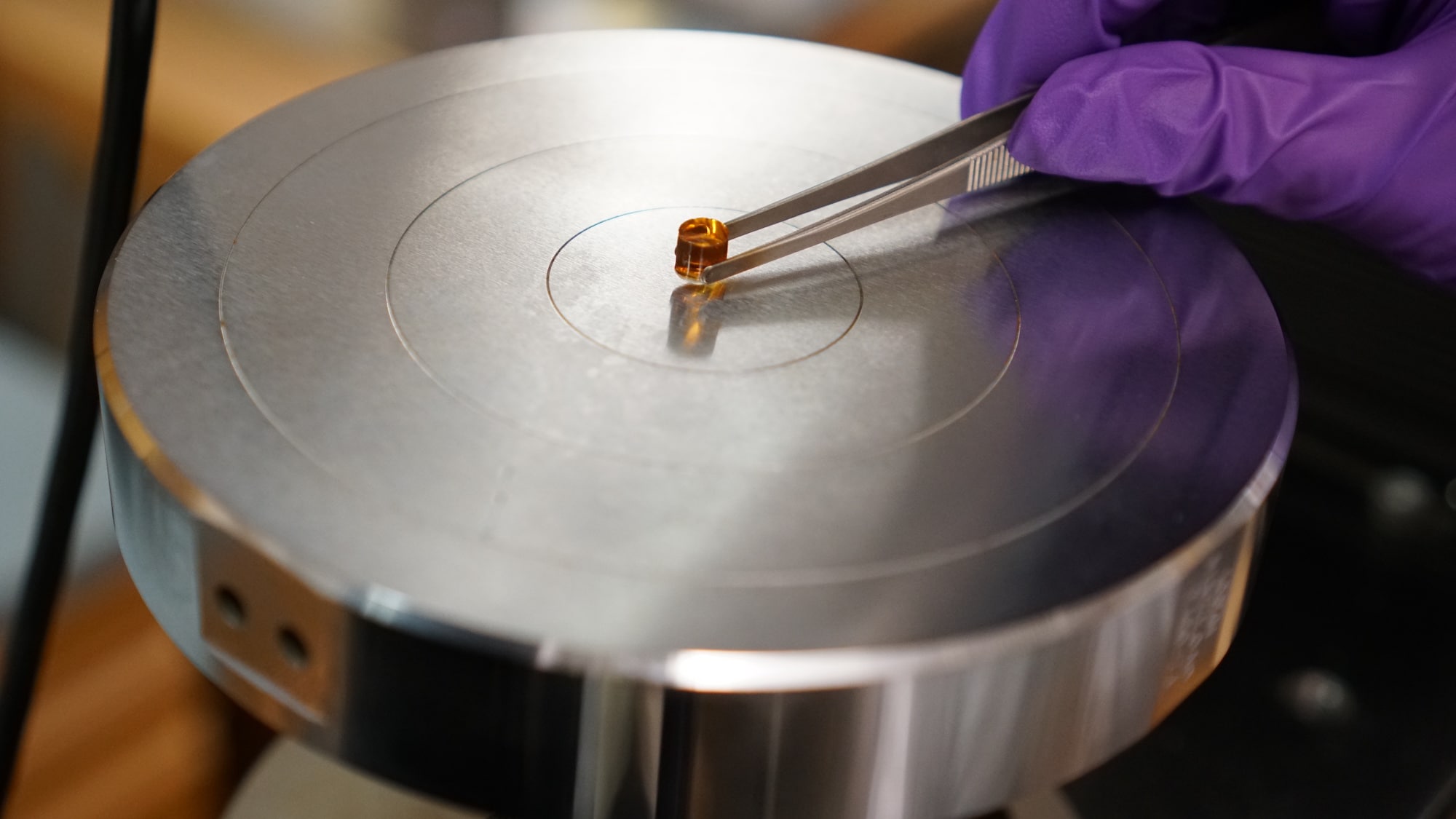
In the study, Dr. Li and his team developed a new approach to stiffen a protein gel without sacrificing toughness, by physically tangling together the chains of a particular protein that made up the gel’s network. “These entangled chains can move, which allows energy, for instance, the impact from jumping, to be dissipated, just like shock absorbers in bikes. In addition, we combined this with an existing method of folding and unfolding proteins, which also allows for energy dissipation,” says first author Dr. Linglan Fu, who conducted the research as a doctoral student at UBC’s Department of Chemistry.
The resulting gel was super tough, able to resist slicing with a scalpel, and was more stiff than other protein hydrogels. Its ability to resist compression was among the highest achieved by any such gels and compared favorably with actual articular cartilage. And the gel was able to rapidly recover its original shape after compression, as real cartilage does after jumping.
Rabbits implanted with the gel showed notable signs of repair of articular cartilage 12 weeks after implantation, with no hydrogel remaining and no rejection of the implant by the animals’ immune system. The researchers observed bone tissue growth similar to the existing tissue, and regenerated tissue close to existing cartilage for the gel implant group—much better results than they saw with a control group.
Interestingly, a stiffer version of the gel had better results than a softer version, likely due to the higher stiffness being more compatible with bone and cartilage tissues, and so providing a physical cue to the body for effective regeneration. However, there can be such a thing as too stiff: the stiffest gel did not work as well, likely due to its slower degradation in the body, the researchers said. “This just shows how complex this area of research is, and the need to take into account the many different physical and biochemical cues and factors when designing these scaffolds,” says co-author Dr. Qing Jiang, a professor and surgeon at Nanjing University.
Further animal testing is needed and the research is still premature for human trials. The researchers’ next steps include this testing, fine-tuning the current gel composition and adding additional biochemical cues to further promote cell regeneration. “By optimizing both biochemical and biomechanical cues together, we will see in the future whether these new scaffolds can lead to even better outcomes,” Dr. Li says.