Materials science pioneer Samuel Stupp believes the future of regenerative medicine may be here sooner than we think. Concepts born in movies — operating suites equipped with 3D printers, lab-grown human tissue, and implanted neurons — are now finding origins in Northwestern laboratories.
Imagine if surgeons could transplant healthy neurons into patients living with neurodegenerative diseases or brain and spinal cord injuries. And imagine if they could “grow” these neurons in the laboratory from a patient’s own cells using a synthetic, highly bioactive material that is suitable for 3D printing.
By discovering a new printable biomaterial that can mimic properties of brain tissue, Northwestern University researchers are now closer to developing a platform capable of treating neurodegenerative diseases or brain and spinal cord injuries using regenerative medicine.
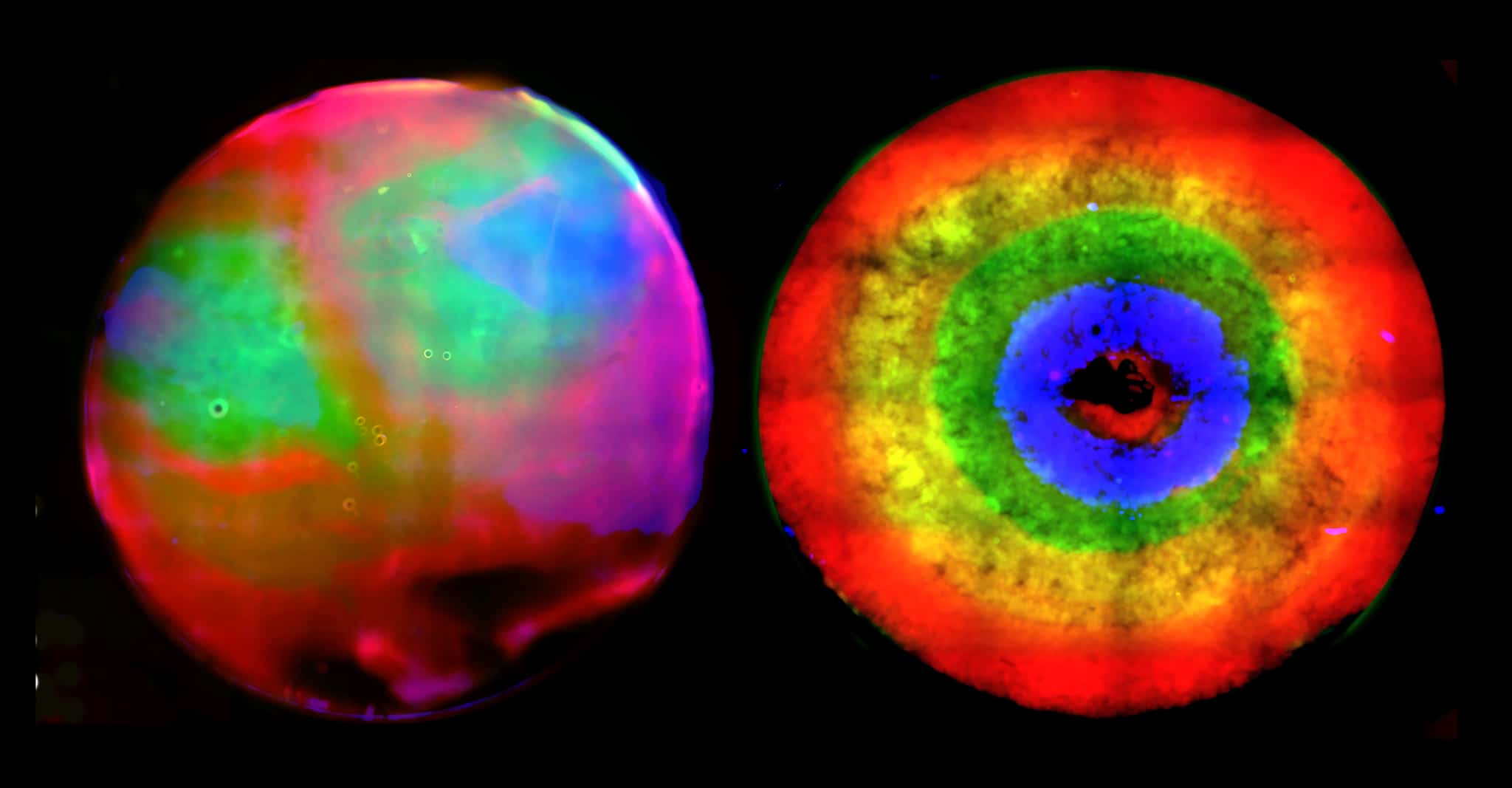
A key ingredient to the discovery is the ability to control the self-assembly processes of molecules within the material, enabling the researchers to modify the structure and functions of the systems from the nanoscale to the scale of visible features. The laboratory of Samuel I. Stupp published a 2018 paper in the journal Science which showed that materials can be designed with highly dynamic molecules programmed to migrate over long distances and self-organize to form larger, “superstructured” bundles of nanofibers.
Now, a research group led by Stupp has demonstrated that these superstructures can enhance neuron growth, an important finding that could have implications for cell transplantation strategies for neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease, as well as spinal cord injury.
“This is the first example where we’ve been able to take the phenomenon of molecular reshuffling we reported in 2018 and harness it for an application in regenerative medicine,” said Stupp, the lead author on the study and the director of Northwestern’s Simpson Querrey Institute. “We can also use constructs of the new biomaterial to help discover therapies and understand pathologies.”
Implications for neurodegenerative diseases and spinal cord injury
According to new research published in the journal Advanced Science, superstructures formed in the Stupp lab can enhance neuron growth, an important finding that could have implications for cell transplantation strategies for neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease, as well as spinal cord injury.
But this research has been almost 20 years in the making, when Stupp first began interacting with biomaterials like these. His lab originally published a paper in 2018 in the journal Science which introduced the dynamic nature of molecules. The agile molecules cover a distance thousands of times larger than themselves in order to band together into large superstructures. At the microscopic scale, this migration causes a transformation in structure from what looks like an uncooked chunk of ramen noodles into ropelike bundles.
Stupp’s team discovered in the new work that when the molecules band together into superstructures, it also leads to the spontaneous formation of pores that are large enough to usher neurons into a nurturing environment in which they can thrive. Putting together three or four different concepts that had their genesis in the same lab, the team created a system they believed could be applied to different tissues throughout the body.
“Still 20 years later, we’re discovering new things with our platform of bioactive materials,” Stupp said.
Tristan Clemons, a research associate in the Stupp lab and co-first author on the paper with Alexandra Edelbrock, a former graduate student in the group, has been studying the material for three years. He said even two years ago, he didn’t appreciate what the superstructure formation could mean.
“Typical biomaterials used in medicine like polymer hydrogels don’t have the capabilities to allow molecules to self-assemble and move around within these assemblies,” said Clemons. “This phenomenon is unique to the systems we have developed here.”
Now that the team has applied a proof of concept to neurons, Stupp believes he could break into other areas of regenerative medicine by applying different chemical structures to the novel biomaterials. Simple chemical changes in the biomaterials would allow them to provide signals for a wide range of tissues.