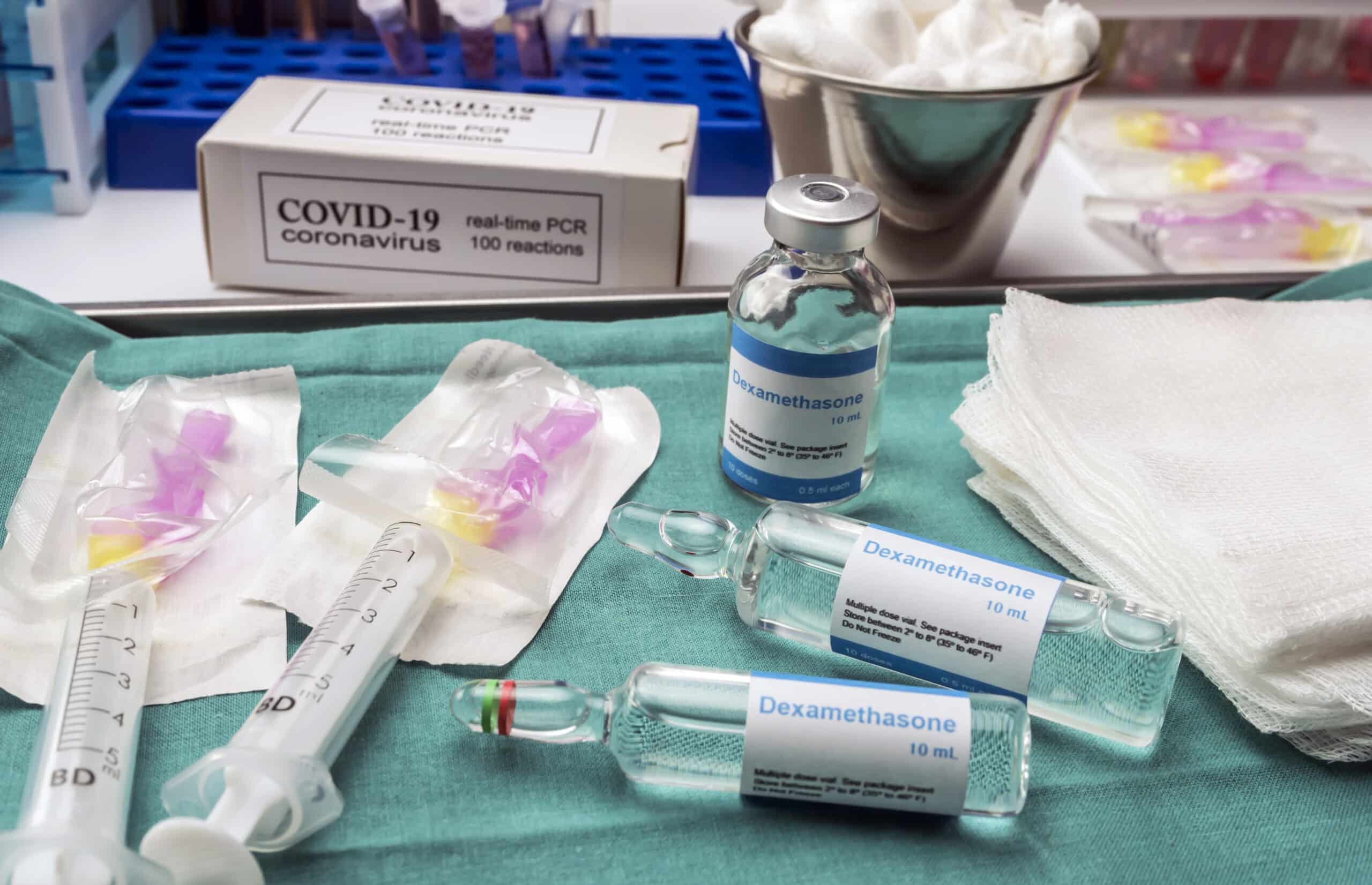
The steroid dexamethasone was found to reduce the risk of death by one third for patients on ventilators and reduced the risk of death by one fifth for patients on oxygen, according to a BBC News Report. The researchers suggest that if this drug had been used from the beginning of the pandemic as many as 5,000 UK lives could have been saved.
“This is the only drug so far that has been shown to reduce mortality — and it reduces it significantly,” chief investigator professor Peter Horby told BBC News. “It’s a major breakthrough.”
As reported on Oxford News:
“A total of 2104 patients were randomised to receive dexamethasone 6 mg once per day (either by mouth or by intravenous injection) for ten days and were compared with 4321 patients randomised to usual care alone. Among the patients who received usual care alone, 28-day mortality was highest in those who required ventilation (41%), intermediate in those patients who required oxygen only (25%), and lowest among those who did not require any respiratory intervention (13%).”
“Dexamethasone reduced deaths by one-third in ventilated patients (rate ratio 0.65 [95% confidence interval 0.48 to 0.88]; p=0.0003) and by one fifth in other patients receiving oxygen only (0.80 [0.67 to 0.96]; p=0.0021). There was no benefit among those patients who did not require respiratory support (1.22 [0.86 to 1.75; p=0.14).”
“Based on these results, 1 death would be prevented by treatment of around 8 ventilated patients or around 25 patients requiring oxygen alone.”
According to Peter Horby, Professor of Emerging Infectious Diseases in the Nuffield Department of Medicine, University of Oxford, and one of the Chief Investigators for the trial, said, “Dexamethasone is the first drug to be shown to improve survival in COVID-19. This is an extremely welcome result. The survival benefit is clear and large in those patients who are sick enough to require oxygen treatment, so dexamethasone should now become standard of care in these patients. Dexamethasone is inexpensive, on the shelf, and can be used immediately to save lives worldwide.”
“Since the appearance of COVID-19 six months ago, the search has been on for treatments that can improve survival, particularly in the sickest patients. These preliminary results from the RECOVERY trial are very clear – dexamethasone reduces the risk of death among patients with severe respiratory complications. COVID-19 is a global disease – it is fantastic that the first treatment demonstrated to reduce mortality is one that is instantly available and affordable worldwide,” said Martin Landray, Professor of Medicine and Epidemiology at the Nuffield Department of Population Health, University of Oxford, who is also one of the Chief Investigators.
“This is tremendous news today from the Recovery trial showing that dexamethasone is the first drug to reduce mortality from COVID-19. It is particularly exciting as this is an inexpensive widely available medicine. This is a ground-breaking development in our fight against the disease, and the speed at which researchers have progressed finding an effective treatment is truly remarkable. It shows the importance of doing high quality clinical trials and basing decisions on the results of those trials,” adds Sir Patrick Vallance who is the UK Government’s Chief Scientific Adviser.
This finding is part of the larger RECOVERY clinical trial that is funded by NIHR. Dexamethasone has been used for over 50 years to treat inflammatory conditions, and in the case of COVID-19 it helps to prevent tissue damage that is caused when the immune system overreacts to the virus in a cytokine storm.
“What this is effectively doing is tamping down inflammatory responses in patients,” Stuart Neil, a professor of virology at King’s College London, told The New York Times. “It’s almost certain this is affecting the body’s response against the virus, rather than inhibiting the virus itself.”
However, it was noted that the drug did not help those who did not require oxygen, and it was not tested on those in home quarantine. This drug should not be administered at home for this use, it should be done in a hospital setting when appropriate, says Landray. “The treatment is up to 10 days of dexamethasone and it costs about £5 per patient,” Landray told BBC News. “So essentially it costs £35 to save a life.”
Still some are skeptical, thinking this may be a redux of HCQ and are taking a contrarian stance on the well known safety profile of the drug tested in a solid study design, but has yet to be peer reviewed. “It will be great news if dexamethasone, a cheap steroid, really does cut deaths by 1/3 in ventilated patients with COVID19, but after all the retractions and walk backs, it is unacceptable to tout study results by press release without releasing the paper,” writer and surgeon Atul Gawande tweeted.
Even some of South Korea’s health officials are urging caution in prescribing the drug due to possible side effects, along with several American physicians being vocal about waiting for a peer reviewed article before making any final judgements, be it positive or negative.
“We have been burned before, not just during the coronavirus pandemic but even pre-COVID, with exciting results that when we have access to the data are not as convincing,” Dr. Kathryn Hibbert, who directs the medical intensive care unit at Harvard’s Massachusetts General Hospital, told Reuters.